What Is Cervical Cancer?
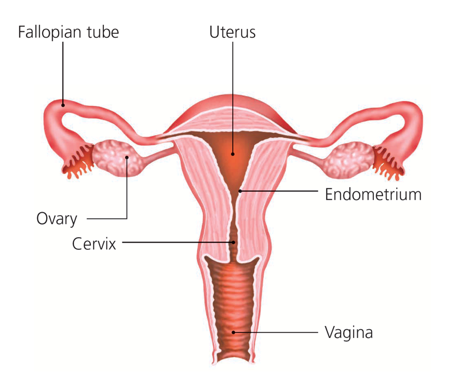
The cervix is inside your vagina at the lower end of your womb (uterus). It is often called the neck of the womb because it is the opening to the womb from the vagina. The cervix is shaped like a cone and is about 2.5 cm (1 inch) long.
Cervical cancer is when normal cells in the lining of your cervix grow in an abnormal way to form a mass of cells called a tumour.
Cervical cancer develops slowly over a number of years, first becoming precancerous and then leading to cancer itself. The precancerous cells may also be called cervical intraepithelial neoplasia (CIN). These cells are not cancerous, but if left untreated may develop into cancer.
How Can I Reduce The Risk of Cervical Cancer?
Have regular cervical screening tests
This can help to spot any changes to cervical cells before they turn cancerous. The national screening programme in Ireland is called CervicalCheck and is available to women aged 25-60. It is free of charge. Learn more about screening here.
Don’t smoke
Not smoking will make it easier for your body to fight an HPV infection and reduce the risk of cancerous changes in the cells in your cervix.
Get vaccinated against HPV
The HPV vaccine protects girls from developing cervical cancer when they are adults. This is why the HPV vaccine is offered to all girls in first year in second level schools to protect them from cervical cancer in adulthood.
Visit www.HPV.ie for more information about HPV.
How Is Cervical Cancer Diagnosed?
Your family doctor (GP) will talk to you about your symptoms and / or your cervical screening test results. They may do some tests. For example:
Cervical examination
An instrument called a speculum is gently put into your vagina (like when you have a cervical screening test) so that the doctor can look at your cervix.
Internal examination
The doctor puts a gloved finger into your back passage or vagina. This because the cervix is close to the bowel and womb, so there may be changes to these parts of the body if you have cervical cancer.
Your GP will refer you to hospital if they think you need more tests. Other tests you might have include:
Using a bright light and a colposcope to look at your cervix. A colposcope is a large magnifying glass or binoculars that helps the doctor to look more closely at the surface of your cervix. This test is done in hospital.
Examination under anaesthetic (EUA)
In this test your doctor can closely examine your cervix and pelvic organs while you are asleep under general anaesthetic. Your doctor can check the size of your womb and if the cancer is found only in your cervix. This test is not always done.
Biopsy
A sample of the cells is taken and looked at under a microscope in the lab to see if there are any cancer cells. The biopsy can be done during a colposcopy or as part of the EUA.
What Are The Stages Of Cervical Cancer?
Staging means finding out the size of the tumour and seeing if it has spread to other parts of the body.
Stage 0 Precancerous cells are found in the surface layer of the cervix only.
Stage 1 Cancer cells are found in the cervix only.
Stage 2 Cancer cells have spread to the top of the vagina or side of the cervix.
Stage 3 Cancer cells have spread to the pelvis.
Stage 4 Cancer cells have spread to other body organs and tissues.
What Are The Symptoms Of Cervical Cancer?
Abnormal vaginal bleeding:
- Periods that are heavier and last longer
- Bleeding in between periods
- Bleeding after sex
- Bleeding after the menopause
Vaginal discharge that may smell unpleasant.
Discomfort or pain during sex, or in the pelvic area.
What Should I Do If I Have Symptoms?
If you have any symptoms or changes in your body that you are worried about, it’s important to have them checked by your GP (family doctor). The chances are it will not be cancer. However, getting your symptoms checked is not wasting anyone’s time. The sooner cancer is spotted, the more likely you are to recover from it.
If you don’t have symptoms, we recommend you continue to attend regular cervical screening. You can check that your details are up to date on the cervical screening register here.
What Are The Types Of Cervical Cancer?
Cervical cancers are recognised by how they look under a microscope.
Squamous cell carcinoma is the most common type of cervical cancer. It develops in the thin flat cells called squamous cells, which are found on the surface of your cervix and vagina. These cells are like skin cells.
Cervical adenocarcinomas are less common. They develop in the gland cells that make mucus in the cervical canal. These cells are shaped like columns.
Adenosquamous carcinomas, mixed carcinomas, clear-cell and small-cell carcinomas are rarer forms of cervical cancer.
What Can Cause Cervical Cancer?
There is strong evidence that cancer of the cervix is caused by a virus called the human papilloma virus (HPV). However, cancer of the cervix is not infectious and so cannot be passed on to others. Your risk of cervical cancer is not increased if someone else in your family has had this cancer. Cervical cancer can happen at any age but is more common in women in their 40s and 50s.
Human Papilloma Virus (HPV)
Most people who have sex will have HPV at some point in their lives. Normally, the infection clears up on its own. HPV infections can lead to abnormal changes in the cells of the cervix. Over time some of these changes can turn into cancer.
Smoking
Chemicals in cigarettes can affect how you fight the HPV infection. For this reason, if you smoke you can have trouble getting rid of the HPV infection. Smoking also increases your risk of abnormal changes (CIN) developing in your cervix.
Not having cervical screening
Having regular cervical screening tests can help to find out if you’re at risk and to spot any changes to cervical cells before they turn cancerous.
Risk factors increase your chance of getting cervical cancer. However, having a risk factor doesn’t mean you will get cervical cancer. Sometimes people with no risk factors may get the disease. You can learn more about reducing risks on pages 7-8 of the Irish Cancer Society’s latest information booklet, visible as a pdf below.
Cervical Cancer Treatment
The way cervical cancer is treated mainly depends on:
- The size and stage of your cancer
- The type of cancer
- If it has spread or not
- Your general state of health
- Your age and fertility
Treatments include: surgery, radiotherapy and chemotherapy (chemoradiation), external radiotherapy, internal radiotherapy (brachytherapy) and targeted therapies.
You can find more detailed information about each treatment type, side effects and support here on the Irish Cancer Society’s website.

221+ Patient Support Group thanks the Irish Cancer Society for permission to use the text of their booklet Cervical Cancer, What You Should Know
in addition to text from their web resources available here. Please find their booklet linked below. We acknowledge the contribution of the original authors.
